The IVF journey is a significant emotional and physical experience, and understanding its complexities and myths are very important for empowering individuals. Focusing on gentle activity, self-care, and open communication with healthcare teams can lead the couple to a healthier recovery after IVF process.
The IVF procedure involves fertilizing an egg outside the body in a laboratory. In this process, every step has a specific significance to get successful pregnancy outcome. The steps include stimulation of ovaries, egg retrieval, fertilization of egg and sperm in laboratory conditions, embryo culture, embryo transfer and implantation into the uterus of female partner and finally check pregnancy test. The fertility experts support the process along with medications for ovaries stimulation, egg development monitoring, and preparation of uterine lining for implantation.
Emotional Impact in IVF Journey
The IVF process may cause hopelessness, anxiety, stress, and uncertainty due to numerous appointments, medications, and waiting periods. It can also lead to social isolation and increased risk of mental health issues. Seeking best fertility expert support is very important to overcome the emotional impact on the couple by discussing the myths and facts of the process.
Physical Aspects of IVF
Ovarian stimulation medications can cause side effects like hot flashes, headaches, nausea, breast tenderness, mood swings, discomfort at the time of egg retrieval and embryo transfer. Ovarian Hyperstimulation Syndrome (OHSS), fatigue may be observed due to hormonal fluctuations and emotional stress, and temporary physical restrictions on post-procedure activities. Medications might cause mild abdominal discomfort and nausea.
Discussing the myths of IVf process
Myth 1: Strict Bed Rest is Essential for Implantation
In general, woman believe that lying completely still for extended periods after the embryo transfer is very important for the embryo to implant successfully.
Reality: After embryo transfer, strict bed rest is not beneficial and may disturb your physical and mental well-being. It’s recommended to resume normal daily routines and gentle activity. Doctors suggest a short rest period of rest for comfort, but prolonged bedtime does not improve pregnancy rates. Implantation is primarily influenced by embryo quality and implantation of embryo in uterus. The bed rest is recommended only to the female partner having history of miscarriages or with low level placenta.
Myth 2: Donor sperms or donor eggs are used in IVF process
Some people believe that IVF involves the use of donor sperm or donor eggs for fertilization.
Reality: In the majority of the IVF cycles, eggs and sperm of the intended couples are used. Donor sperm, donor eggs, or donor embryos are used only in specific situations, such as when one or both partners have significant fertility issues, genetic concerns, or have had multiple failed IVF cycles with their own egg or sperm. The decision to use donor materials is taken by the individual couple, made in consultation with a fertility specialist.
Myth 3: Baby is born with abnormalities when conceived by IVF process
There’s a misconception that IVF procedures increase the risk of birth defects or developmental abnormalities in babies.
Reality: IVF babies have a similar risk of major birth defects to naturally conceived babies (3 to 4 %), with advanced maternal age being a significant factor. Preimplantation Genetic Testing (PGT) is often used to screen embryos for specific genetic disorders before transfer, potentially reducing the risk of passing on inherited conditions.
Myth 4: Caesarean Section is Mandatory for IVF Pregnancies
Some couple believe that all pregnancies achieved through IVF need a C-section for delivery.
Reality: A C-section is not mandatory for IVF-conceived pregnancies. The mode of delivery is determined by the same factors as naturally conceived pregnancies. It includes the mother’s and baby’s health, baby’s position, and labor complications at the time of delivery. Many IVF-conceived women have successful vaginal deliveries.
Myth 5: IVF Almost Always Results in Multiple Pregnancies (Twins, Triplets, etc.)
There’s a common perception that IVF frequently leads to multiple pregnancies, especially twins.
Reality: IVF has a higher risk of multiple pregnancies compared to natural conception due to the historical practice of transferring multiple embryos. However, modern IVF is focusing on elective single embryo transfer (eSET), which significantly reduces the risk of high-order multiple pregnancies and complications associated with twin pregnancies. While twins can still occur with eSET, it’s less common than transferring multiple embryos.
Myth 6: The IVF Procedure is Extremely Painful!
Many individuals fear that the IVF process, particularly egg retrieval and embryo transfer, is intensely painful.
Reality: The IVF process is a minor procedure that includes: egg retrieval, performed under sedation or anesthesia, is painless and can sometimes cause mild cramping or discomfort. Embryo transfer is a quick, painless procedure and can also be done under sedation if necessary. Over-the-counter pain relievers can manage the minimal pain caused by the procedure.
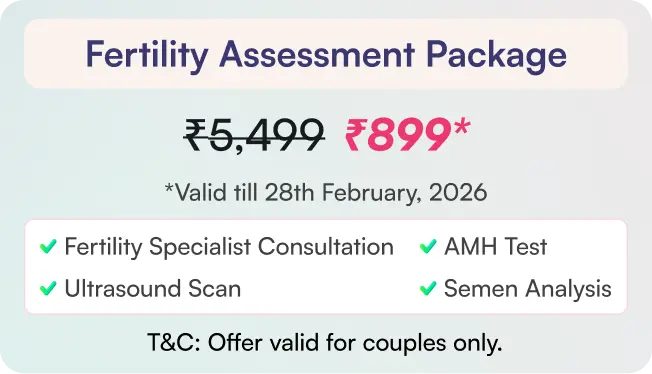
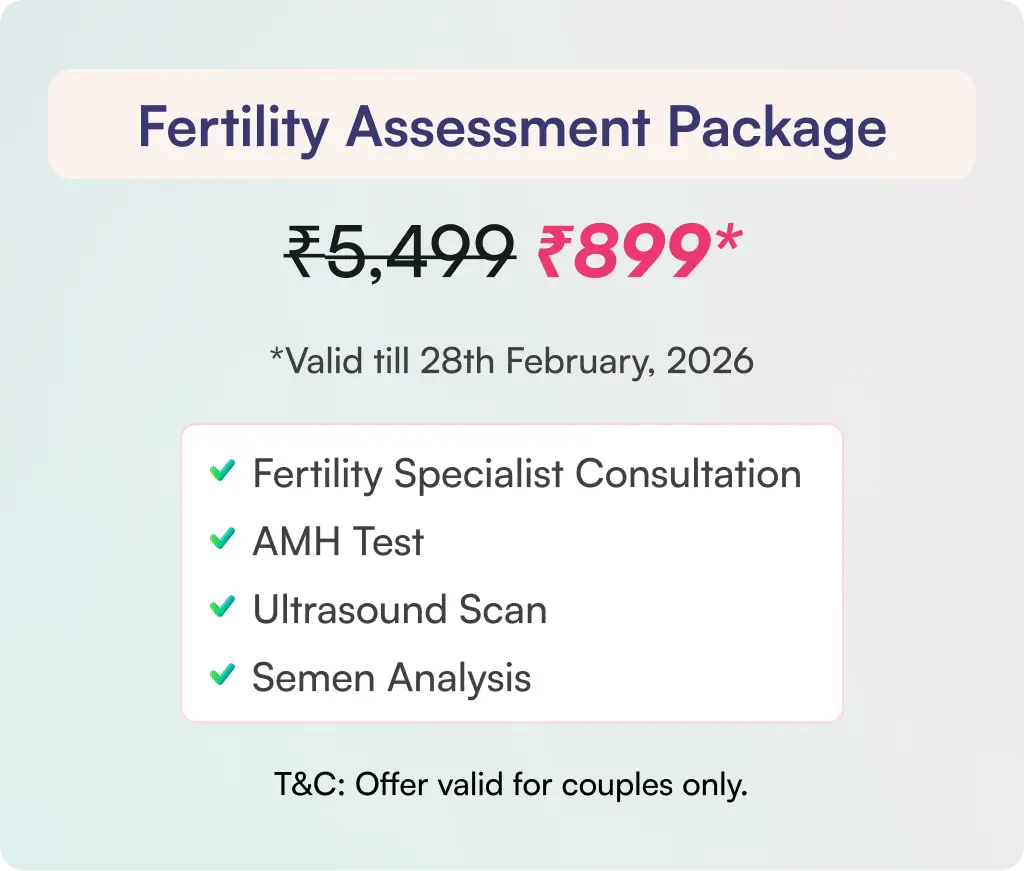
Myth 7: IVF is a costly treatment option, making it unaffordable for most individuals and couples experiencing infertility
Reality: The cost of IVF procedure is based on factors like quality of the treatment, number of eggs and embryo with high quality, the number of cycles needed, the medications used for ovarian stimulation, and involvement of additional procedures like ICSI, PGT, embryo freezing, and storage. Based on the complication associated and the condition of the partners the cost will differ.
Myth 8: Individuals often worry about the risk of increase in ovarian cancer due to the use of ovarian stimulation drugs in IVF process.
Reality: IVF process does not increase the risk of ovarian cancer. The primary risk factors are similar as in the normal people with a family history or any exposures to harmful chemicals that cause cancer. The fertility medications used in IVF are generally safe in the long term.
Myth 9: Some believe that once conceiving through IVF, the future pregnancies will also require IVF treatment.
Reality: A successful IVF cycle will not require future pregnancies should follow the same procedure. Factors influencing this include the underlying cause of infertility, lifestyle changes and medical management, and the success of IVF resetting the reproductive system. In some cases, the factors that initially led to infertility may improve over time or resolve spontaneously. managing lifestyle changes and improvements in underlying medical conditions can lead to natural fertility.
Conclusion:
IVF treatment involves fertilizing an egg outside the body in a laboratory, causing emotional and physical changes in individuals. However, understanding the myths of IVF procedure may help the couple understand better and focus on gentle activity, self-care, and open communication and may lead to a healthier recovery after IVF process.