What is Spermatogenesis?
Spermatogenesis, also known as the sperm regeneration cycle, is the intricate biological process by which male reproductive cells, called spermatozoa or sperm, are produced. This complex process occurs continuously in the testes of sexually mature men, ensuring a steady supply of sperm for fertilisation.
Spermatogenesis is a highly regulated and efficient process that involves the division and differentiation of specialised cells called spermatogonial stem cells. These stem cells undergo a series of transformations, ultimately forming mature, motile sperm capable of fertilising an egg.
The sperm regeneration cycle is crucial for male fertility and vital to human reproduction. Understanding this process is crucial for maintaining optimal reproductive health and addressing potential fertility issues.
Related Read: AndroMax: Ferty9’s Solution for Enhancing Male Fertility
Where Does Sperm Production Occur?
Sperm production primarily occurs within the seminiferous tubules, which are tightly coiled structures in the testes (testicles). These tubules provide the ideal environment for spermatogenesis, with specialised cells called Sertoli cells playing a supportive role in nurturing and protecting the developing sperm cells.
The testes are in the scrotum, a pouch-like structure hanging outside the male body. The scrotum’s unique position helps regulate the temperature required for optimal sperm production, as sperm cells are sensitive to temperature fluctuations.
In addition to the seminiferous tubules, other structures within the testes, such as the Leydig cells, play an elementary role in the hormonal regulation of spermatogenesis.
Also read: Effective Methods of Treating Male Infertility
Key Hormones Involved in Sperm Production
Spermatogenesis is a hormonally controlled process, with several hormones playing critical roles in regulating and maintaining sperm production. The primary hormones involved are:
- Gonadotropin-releasing Hormone (GnRH): Produced by the hypothalamus, GnRH signals the pituitary gland to secrete two other essential hormones, Luteinising Hormone (LH) and Follicle-stimulating Hormone (FSH).
- Luteinising Hormone (LH): Produced by the pituitary gland, this hormone triggers the Leydig cells in the testes to synthesise testosterone hormone.
- Follicle-stimulating Hormone (FSH): Also released by the pituitary gland, FSH acts on the Sertoli cells in the seminiferous tubules, promoting the growth and development of sperm cells.
- Testosterone: The primary male sex hormone secreted by the Leydig cells in response to LH, testosterone plays a vital role in initiating & maintaining spermatogenesis and supporting the development of male reproductive organs and secondary sexual characteristics.
These hormones work in a coordinated manner, forming a complex feedback loop that ensures the proper regulation of sperm production.
Also read: Did You Know 1 in 6 People Globally Are Affected by Infertility?
The Stages of the Sperm Regeneration Cycle
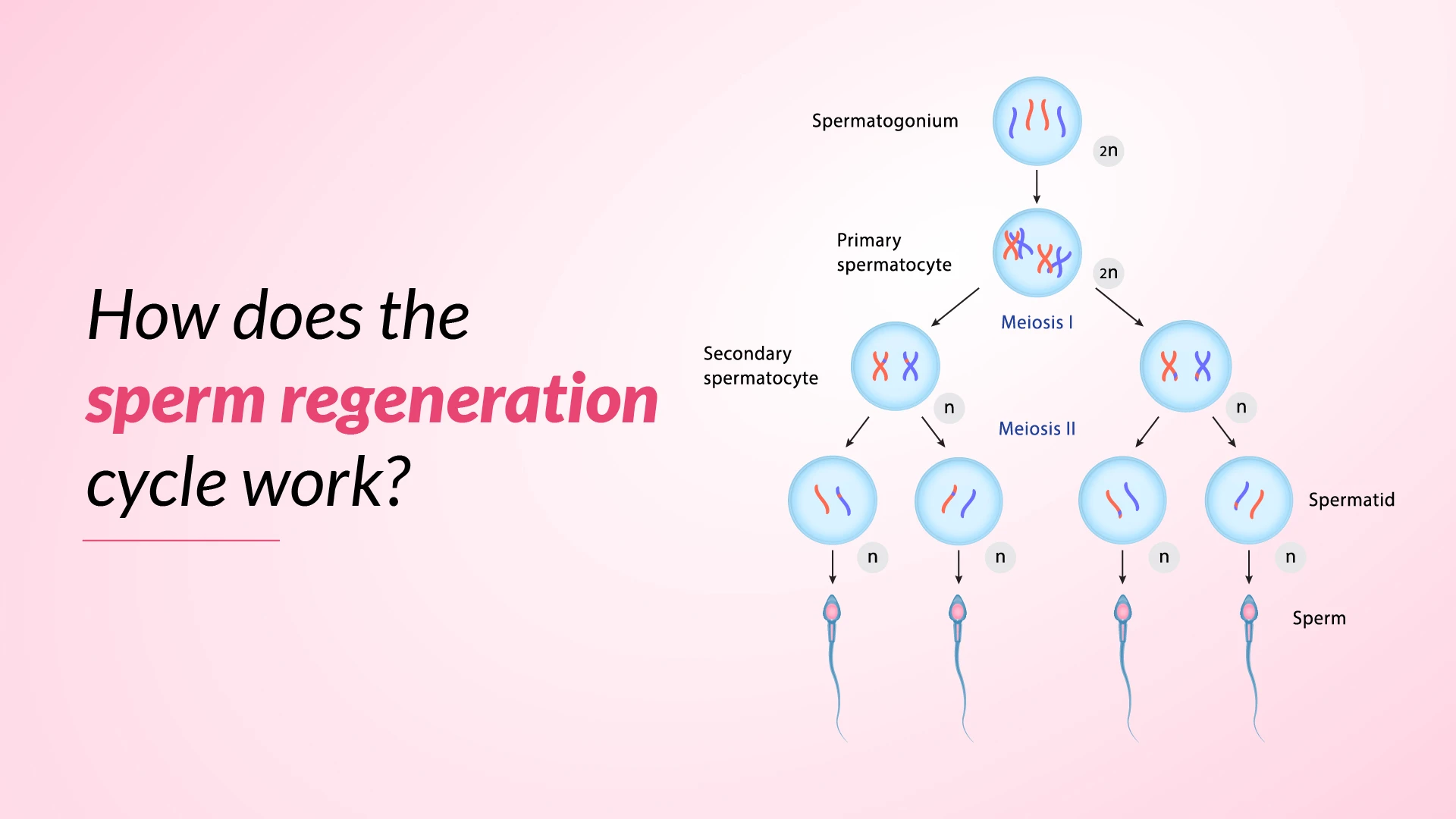
The sperm regeneration cycle, or spermatogenesis, consists of four distinct stages:
Stage 1: Spermatocytogenesis
Spermatocytogenesis is the initial stage of spermatogenesis, during which spermatogonial stem cells undergo several rounds of mitotic division, increasing their numbers. Some of these cells remain stem cells, while others differentiate into primary spermatocytes, larger cells with double the genetic material (diploid). This process takes place within the seminiferous tubules of the testes.
Stage 2: Meiosis
The second stage of spermatogenesis is meiosis, a specialised cell division type that reduces the number of chromosomes in the cells from diploid (46 chromosomes) to haploid (23 chromosomes). This process ensures that the resulting sperm cells carry only half the genetic material, allowing for the proper combination of genetic material during fertilisation.
During meiosis, the primary spermatocytes undergo two consecutive cell divisions, known as meiosis I and meiosis II, forming four haploid spermatids from each primary spermatocyte.
Stage 3: Spermiogenesis
Spermiogenesis is the third stage of spermatogenesis, during which the haploid spermatids undergo a remarkable transformation to become mature, motile sperm cells. This process involves several morphological changes, including developing a compact nucleus, the formation of a flagellum (tail) for motility, and condensing genetic material.
During spermiogenesis, the spermatids undergo a series of structural and biochemical modifications, shedding excess cytoplasm and developing specialised organelles, such as the acrosome, which plays a crucial role in fertilisation.
Stage 4: Spermiation
The final stage of spermatogenesis is spermiation, during which the fully formed, mature sperm cells are released from the seminiferous tubules into the lumen (interior space) of the tubules. This process involves the detachment of the sperm cells from the Sertoli cells, which have nurtured and supported their development.
Once released, the sperm cells undergo further maturation and capacitation as they travel through the epididymis, a coiled tubular structure adjacent to the testes. This process prepares the sperm cells for fertilisation by enabling their motility and enhancing their ability to penetrate and fertilise an egg.
Also read: Is Male Fertility Higher or Lower Compared to Female Fertility?
Factors Affecting Sperm Regeneration
While spermatogenesis is a highly regulated process, various factors can influence sperm production and quality, including:
Age and Sperm Production:
As men age, their sperm production and quality may gradually decline. This is due to a combination of factors, including hormonal changes, decreased testicular function, and the accumulation of genetic mutations over time.
Diet and Nutrition:
A balanced & nutrient-rich diet is key for optimal sperm production and quality. Certain nutrients, such as zinc, vitamin C, vitamin E & omega-3 fatty acids, play essential roles in supporting spermatogenesis and sperm health.
Exercise and Physical Activity:
Regular moderate exercise can positively impact sperm production and quality, as it promotes overall health and helps regulate hormonal levels. However, excessive or intense exercise can potentially negatively affect sperm regeneration.
Exposure to Toxins and Chemicals:
Exposure to certain environmental toxins (pesticides, heavy metals, and industrial chemicals) can adversely affect sperm production and quality. These substances can disrupt hormonal balance & contribute to oxidative stress, potentially damaging sperm cells.
Heat and Radiation:
The testes are sensitive to temperature fluctuations, and prolonged exposure to high temperatures, such as those experienced during sauna use or prolonged sitting with a laptop on the lap, can impair sperm production. Similarly, exposure to ionising radiation can also have detrimental effects on spermatogenesis.
Medical Conditions and Medications:
Certain medical conditions, such as diabetes, cancer, and hormonal imbalances, can impact sperm production and quality. Additionally, some medications, including chemotherapeutic agents, anabolic steroids, and certain antidepressants, can interfere with spermatogenesis.
Also read: The Impact of Stress on Men’s and Women’s Sexual Health
Maintaining Healthy Sperm Production
To support optimal sperm production and overall reproductive health, men can adopt certain lifestyle practices:
- Maintain a Healthy Diet Schedule: Consume a balanced diet rich in nutrients like zinc, vitamins C and E, and omega-3 fatty acids, essential for sperm health.
- Exercise Regularly: Engage in moderate physical activity to promote overall health & maintain a healthy weight, as obesity can negatively impact sperm production.
- Manage Stress: Chronic stress can disrupt hormonal balance and impair sperm production. Practice stress-management techniques like meditation, yoga, or deep breathing exercises.
- Avoid Smoking and Alcohol Consumption: Tobacco smoking & excessive alcohol intake can affect sperm quality and production. Therefore, limit or avoid these illicit habits.
- Limit Exposure to Environmental Chemicals: Minimise exposure to pesticides, heavy metals, and other environmental pollutants to improve sperm health.
- Maintain a Healthy Weight: Being overweight or obese can contribute to hormonal disparities and negatively impact sperm production. Therefore, maintaining optimal body weight is crucial for better sperm quality and production.
- Seek Medical Advice: If you are facing fertility problems or have concerns about your sperm health, consult with a professional for proper evaluation and treatment.
Find Hope and Solutions for Female Infertility and Male Infertility — Explore Our Comprehensive Services
IVF Treatment
IUI Treatment
ICSI Treatment
PICSI Treatment
Fertility Preservation Service
Blastocyst Culture & Transfer Treatment
Conclusion
The sperm regeneration cycle, or spermatogenesis, is a complex and regulated process that ensures the continuous production of mature, motile sperm cells. Understanding the intricacies of spermatogenesis and the factors that can influence sperm production is essential for maintaining optimal reproductive health and addressing potential fertility issues. By adopting a healthy lifestyle, handling stress, and seeking medical advice when necessary, men can support their sperm regeneration cycle and increase their chances of achieving successful fertilisation.
Remember, sperm health is a vital component of male fertility, and taking proactive steps to maintain a healthy sperm regeneration cycle can significantly impact your overall reproductive well-being.