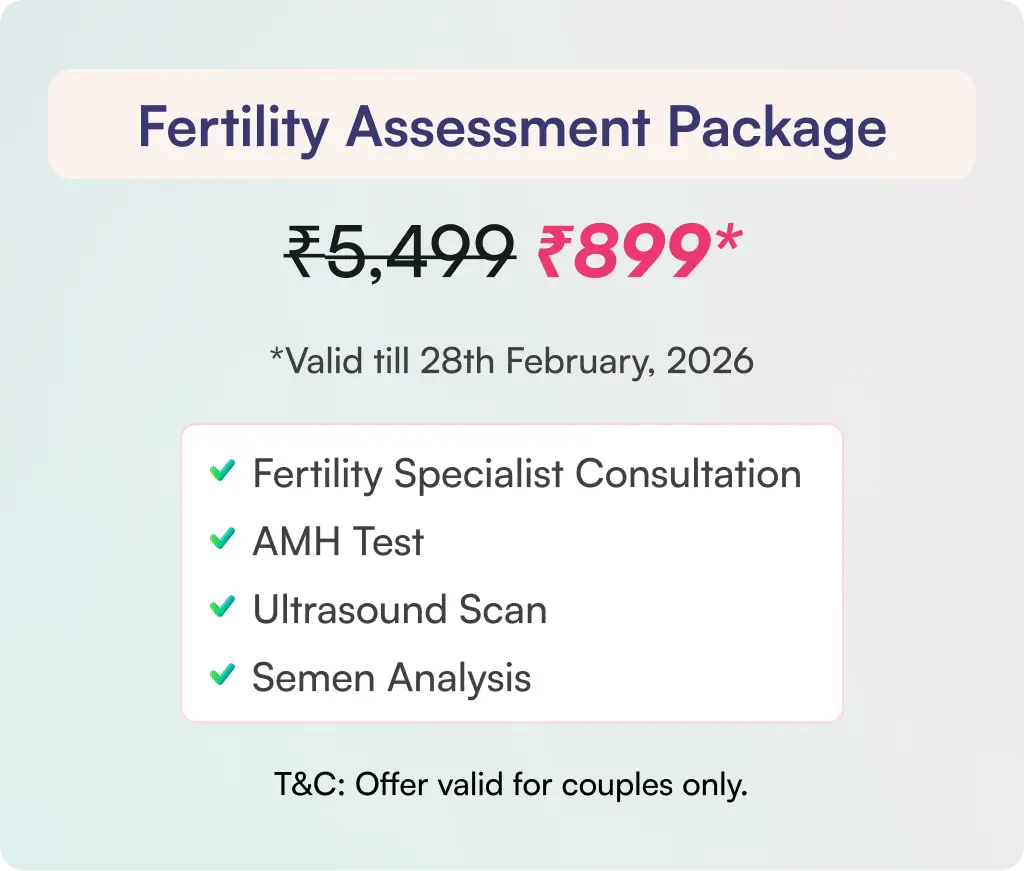
A woman’s ovarian reserve represents her reproductive potential, determining how many eggs she has available for future pregnancies. This biological clock is more complex than age alone, and some women face challenges when their ovarian reserve diminishes earlier than expected. Diminished ovarian reserve (DOR) occurs when the number & quality of eggs in a woman’s ovaries decline, potentially affecting her ability to conceive. While this condition becomes more common with age, it can affect women at any stage of their reproductive years. This comprehensive blog explores the symptoms, causes, and available treatments for diminished ovarian reserve, helping readers understand their options & make informed choices about their reproductive health.
Also read: Ovarian Reserve Decline: A Key Factor in 50-60% of Female Infertility
What are the Signs & Symptoms of Diminished Ovarian Reserve?
Identifying diminished ovarian reserve can be challenging as the condition often develops silently. Most women don’t notice any obvious signs in the early stages, making it essential to understand potential indicators that might signal this condition.
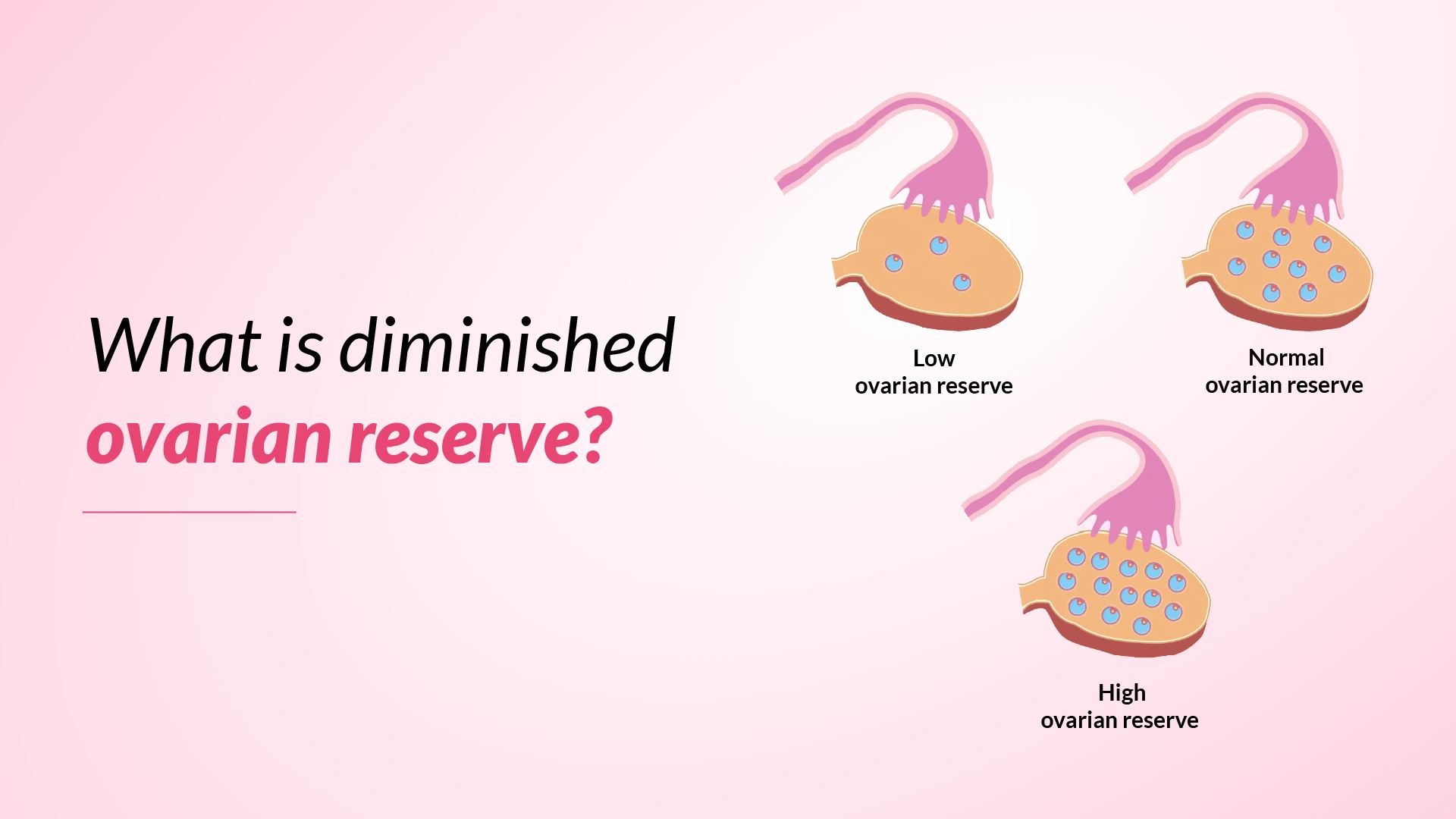
The most noticeable symptom of diminished ovarian reserve is a change in menstrual patterns. Women may observe their cycles becoming shorter, typically shifting from 28 to 24 days. As the condition progresses, several symptoms may become apparent:
- Changes in Menstrual Cycles: Irregular periods or changes in cycle length
- Fertility Challenges: Difficulty conceiving despite regular attempts
- Hormonal Signs: Hot flashes and night sweats
- Sleep Disturbances: Trouble maintaining regular sleep patterns
- Physical Changes: Vaginal dryness and other oestrogen-related symptoms
What Causes Diminished Ovarian Reserve?
The causes of diminished ovarian reserve are diverse and complex, affecting women through various biological and environmental factors. While age remains a significant factor, medical research has identified several other important causes that can impact a woman’s ovarian reserve. Several factors can cause diminished ovarian reserve:
- Medical Conditions: Certain systemic conditions play a crucial role in affecting ovarian reserve. Endometriosis, particularly when accompanied by ovarian cysts, significantly increases the risk of developing diminished ovarian reserve. Women with hypothyroidism also show higher chances of experiencing this condition.
- Genetic Factors: Family history, mainly if the mother or grandmother experienced early menopause
- Medical Procedures: Chemotherapy, radiation therapy, and ovarian surgeries
- Autoimmune Conditions: Conditions like lupus and rheumatoid arthritis
- Environmental Exposure: Contact with certain chemicals, pesticides, and pollutants
- Lifestyle Choices: Smoking and other unhealthy habits
- Occupational Factors: Long working hours, handling heavy objects, and non-daily shift work
Research has also revealed that maternal factors during pregnancy can influence ovarian reserve in offspring. These include exposure to certain substances, maternal nutrition, and socio-economic conditions during pregnancy. Chronic inflammation and exposure to persistent organic pollutants through drinking water and food packaging materials can also affect ovarian reserve.
Screening Tests for Diminished Ovarian Reserve
Modern medical science offers several reliable screening tests to evaluate ovarian reserve, helping doctors assess a woman’s reproductive potential. These tests provide valuable insights into egg quantity and potential fertility treatment outcomes.
The most comprehensive assessment of ovarian reserve involves three primary tests:
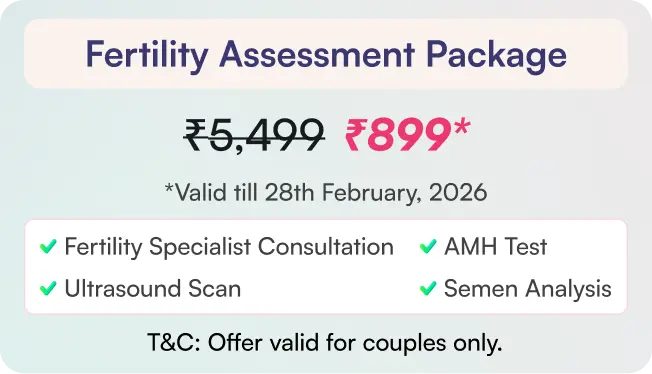
- Anti-Müllerian Hormone (AMH): This blood test measures hormone levels produced by developing egg follicles. AMH levels remain at consistent levels throughout the menstrual cycle, making it a convenient & reliable marker.
- Antral Follicle Count (AFC): Performed via transvaginal ultrasound, this test counts small follicles in both ovaries. Doctors typically conduct this examination during the first four days of the menstrual cycle.
- Follicle Stimulating Hormone (FSH): Measured through a blood investigation on day three of the menstrual cycle, FSH levels above ten mIU/mL may indicate decreased ovarian function.
Among these options, AMH and AFC have emerged as the most sensitive and reliable indicators of ovarian reserve. These tests are particularly valuable for predicting how well a woman might respond to fertility treatments like IVF. Doctors often combine multiple tests to create a comprehensive picture of ovarian reserve, as no single test can definitively predict fertility outcomes. Results should always be interpreted within the context of a woman’s age and overall health profile.
Fertility Treatments for Women with DOR
The treatment choice depends on factors such as age, desired timeline for pregnancy, and personal fertility goals.
Doctors typically recommend several treatment approaches:
- Fertility Preservation: Freezing eggs before further decline in ovarian reserve
- Controlled Ovarian Hyperstimulation: Using hormonal medications to stimulate multiple egg production
- In Vitro Fertilisation (IVF): Collecting and fertilising eggs in a laboratory setting
- Donor Egg Options: Using eggs from a younger donor when necessary
- Embryo Freezing: Creating and preserving embryos for future use
The journey often begins with ovarian stimulation, where hormonal medications help produce multiple eggs in a single cycle. This approach can be combined with intrauterine insemination or IVF depending on individual circumstances.
For women seeking to preserve their fertility, egg freezing presents a proactive solution. This process involves hormone stimulation, egg collection, and cryopreservation for future use. Some patients may opt for embryo freezing, which involves fertilising eggs with a partner or donor sperm before preservation.
When traditional treatments prove challenging, donor eggs offer a viable alternative. While the resulting child won’t share the mother’s genetic material, this option allows women to experience pregnancy and childbirth. Success rates with donor eggs are notably high, providing hope for many couples facing fertility challenges.
How Successful is IVF with Low Ovarian Reserve?
IVF success rates in women with diminished ovarian reserve vary significantly based on several factors, with timing and underlying causes playing crucial roles in treatment outcomes. While the overall statistics might seem challenging, with clinical pregnancy rates around 11.5% per cycle, individual outcomes can differ substantially.
The cause of low ovarian reserve significantly influences IVF success. Women with DOR resulting from previous ovarian surgery often show more promising outcomes compared to other causes. However, those who developed the condition due to chemotherapy or gonadotoxic therapy face higher cycle cancellation rates.
Several factors influence IVF success rates:
- Age of the patient: Younger women with DOR show better outcomes
- Timing of treatment: Earlier intervention typically yields better results
- Cause of the condition: Surgery-related DOR has better pregnancy rates
- Number of eggs retrieved: Even with fewer eggs, quality remains crucial
- Individual response to stimulation: Varies among patients
For younger women with diminished ovarian reserve who proceed to egg retrieval, the prognosis remains encouraging. While they may produce fewer eggs during collection, the embryos they do create show similar implantation rates to those from women with normal ovarian reserve, offering hope for successful pregnancy outcomes.
How Can I Reduce My Risk for Diminished Ovarian Reserve?
While some factors affecting ovarian reserve are beyond control, women can take proactive steps to protect their reproductive health. Making informed lifestyle choices is crucial in maintaining optimal ovarian function and reducing the risk of premature decline.
Key preventive measures that women can implement include:
- Maintaining a healthy BMI through proper nutrition and exercise
- Avoiding tobacco products completely
- Limiting alcohol consumption when trying to conceive
- Keeping caffeine intake below 200 mg daily
- Protecting against environmental toxins, including pesticides and solvents
- Moderating exercise intensity to avoid overtraining
For women undergoing pelvic surgery, particularly for conditions like endometriosis, working with doctors who prioritise ovarian tissue preservation is essential. Special attention should be given during surgical procedures to minimise damage to the ovarian cortex.
Folic Acid to Improve Egg Quality
Folic acid emerges as a crucial nutrient in the quest for optimal egg quality, playing a vital role in cellular DNA synthesis and reproductive health. This B-group vitamin actively participates in the development of oocytes, making it an essential component for women concerned about their fertility.
Research demonstrates that folic acid supplementation offers several significant benefits for egg quality:
- Enhances DNA synthesis in developing eggs
- Improves hormonal balance and follicular development
- Reduces harmful homocysteine levels in follicular fluid
- Supports proper cell division processes
- Helps prevent oxidative stress in developing eggs
Studies indicate that supplemental folic acid intake up to 1200 μg/day shows positive associations with antral follicle count, suggesting improved ovarian function. The absorption rate of supplemental folate significantly exceeds that of food-based sources, making supplements particularly effective for women focusing on fertility enhancement.
Doctors often recommend folic acid supplementation because it works at the cellular level, helping with DNA synthesis, modification, and repair. This becomes especially important for women with diminished ovarian reserve, as the vitamin’s role in cell division and chromosome repair can contribute to better egg quality outcomes.
Find Hope and Solutions for Female Infertility and Male Infertility — Explore Our Comprehensive Services
IUI Treatment
ICSI Treatment
PICSI Treatment
Fertility Preservation Service
Blastocyst Culture & Transfer Treatment
Genetic Screening & Testing
Conclusion
Women diagnosed with diminished ovarian reserve can explore various treatment paths, from fertility preservation to IVF and donor egg options. Success rates vary based on individual factors, but early intervention often leads to better outcomes.
Lifestyle modifications play an elementary role in maintaining ovarian health. Regular exercise, proper nutrition, and folic acid supplementation can help protect egg quality. Women should work closely with doctors to develop personalised treatment strategies that align with their reproductive goals.
The journey through diminished ovarian reserve might seem challenging, but proper medical guidance and proactive health management can significantly improve outcomes. Regular monitoring, lifestyle adjustments, and timely interventions create the best possible environment for reproductive success.