Embryo transfer stage in IVF
Beginning the in vitro fertilization (IVF) journey is full of hope and promise. A vital step in this process is placing embryos in the uterus. This is meant to support a healthy pregnancy. Many couples eagerly question the best number of embryos to transfer. Let’s take a closer look at this important topic. We’ll discuss embryo age, potency, and the factors influencing success rates.
Cleavage-stage embryos are usually transferred 2 to 7 days after egg retrieval. In contrast, blastocysts are transferred 5 to 7 days later.
Number of Embryos Transferred: A Deliberate Decision
This is probably the key point. You should have a detailed discussion with your fertility specialist. It’s not only about improving the chances of pregnancy in a single cycle. It’s also about considering the risks linked to having multiple pregnancies. Here’s a more granular look:
Individualized Assessment: The “ideal” number of embryos to transfer varies for each person. Your doctor will consider several factors specific to your situation:
Age: Younger patients often have higher implantation rates per embryo. This makes single embryo transfer (SET) a better choice. It offers great success rates and reduces the chance of twins. Older patients might want to transfer two embryos. Still, they should think about the risks that come with multiple pregnancies.
- 3-Day Embryos: By now, the embryo has divided a few times. It usually has 6 to 8 cells.
- 5-Day Embryos (Blastocysts): On day 5, the embryo grows into a blastocyst, which is a more complex form.
Embryo Quality: High-quality blastocysts have a significantly higher implantation potential. Transferring one high-quality blastocyst can achieve success rates similar to using multiple lower-quality embryos. This method also reduces the risk of having multiples.
Previous IVF Cycles: If your IVF cycles didn’t work, doctors will look into why they failed. This may affect the decision. The main goal is to transfer no more than 2 embryos. They should have a good chance of success and ensure safety.
Uterine Factors: The condition of your uterus and any history of issues are also important.
Patient Preferences: Though doctor advice is important, your choices and awareness of the risks are important as well.
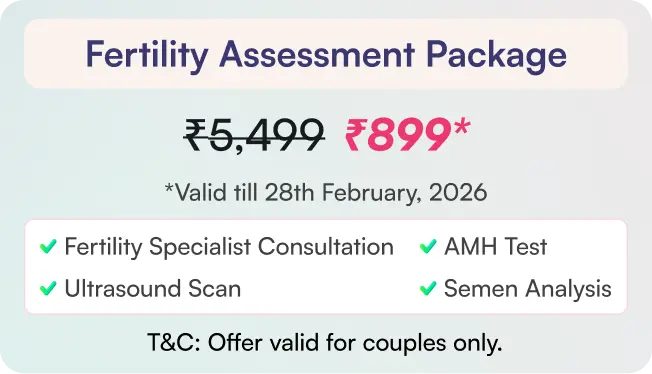
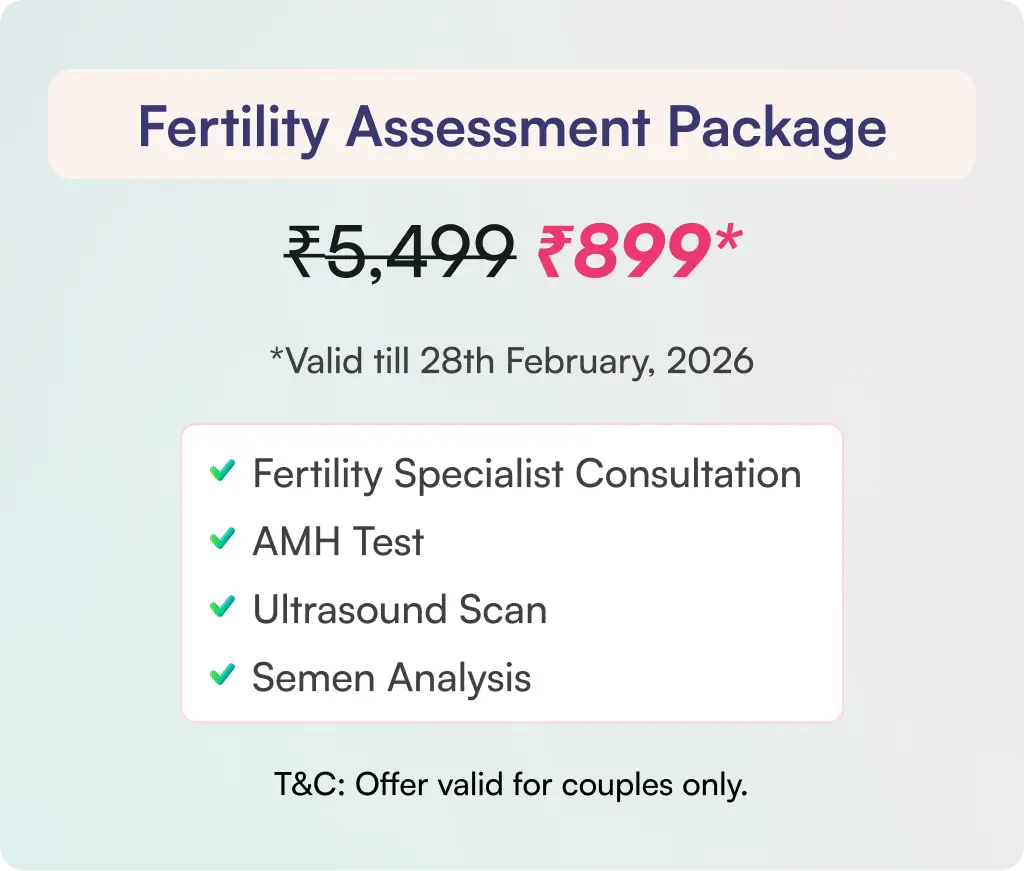
How many embryos can be transferred?
Deciding how many embryos to transfer is important. It balances the wish for pregnancy with the risks of multiple births. The idea of having twins can be exciting. But carrying more than one baby raises the risk of problems for both the mother and the newborns. We prefer to transfer single blastocyst. A maximum of two embryos can be transferred in a single cycle.
The Age Factor: 3-Day vs. 5-Day Embryos (Blastocysts)
Embryos are usually transferred at either the 3-day stage or the 5-day stage. This is when they become blastocysts. This age difference is significant:
Why are 5-day embryos selected?
Blastocysts are generally considered more potent than 3-day embryos for several reasons:
Natural selection: Embryos that reach the blastocyst stage can develop better. Some embryos stop growing before reaching this stage. Transferring a blastocyst enables the natural process to take a major role. This could improve the chances of implantation.
Improved Timing: A 5-day blastocyst aligns well with the uterine environment. The uterus is generally more prepared for implantation at this point.
Higher success rates: Blastocysts implant better than 3-day embryos during transfers.
Impact on success rates based on embryo age
The success rate of IVF resulting in a live birth depends on several factors. Key factors include the woman’s age, the quality of embryos, and the number transferred. It might seem that transferring more embryos would improve pregnancy chances. It can significantly increase the risk of multiple pregnancies.
For blastocyst transfers, doctors can transfer one embryo (SET) or two embryos. Transferring two usually leads to better success rates. Three-day embryo transfer may not be as successful compared to a 5-day embryo. This is due to the increased viability and implantation potential of blastocysts.
Prioritizing Mother and Child Health
The government understands the risks of multiple pregnancies, such as triplets or more. They often have rules about how many embryos can be transferred. A common rule is to transfer no more than two blastocyst embryos in one cycle. This regulation works to lower the chances of having triplets and other risky multiple pregnancies. It focuses on the health and well-being of both the mother and the children. Doctors and fertility experts recommend transferring no more than two embryos. This helps reduce health risks for both the mother and the baby.
The Risks of Transferring Three Blastocysts
Transferring three blastocysts significantly increases the likelihood of a triplet pregnancy. Having three babies at once can seem like a joy, but it comes with serious risks, including:
Increased risk of preterm birth: Premature babies often face significant health challenges.
Higher rates of low birth weight: This can lead to developmental issues.
Mothers can encounter more complications: These may include gestational diabetes, preeclampsia, and the possibility of needing a Cesarean section.
Considering Two Embryo Transfers
Fertility experts mostly favor single embryo transfer (SET), particularly when using high-quality blastocysts. The goal is a healthy singleton pregnancy. This type of pregnancy leads to the best outcomes for both the mother and the baby. In case of two embryos, the risk of twins will be present.
Conclusion:
When it comes to embryo transfer in IVF, the focus is more on quality than quantity. Transferring one high-quality blastocyst gives a good chance of having one baby. This also lowers the risks linked to having twins or more. Keeping both mother and child healthy during pregnancy is the most important thing. Discuss your situation with your fertility specialist. This helps find the safest and best embryo transfer plan for you.