Embryo grading in IVF is a crucial step where embryologists assess lab-created embryos. This careful evaluation finds those most likely to have successful implantation and pregnancy. Choosing the right embryos during transfer can improve the chances of getting pregnant.
Important stages of embryo transfer
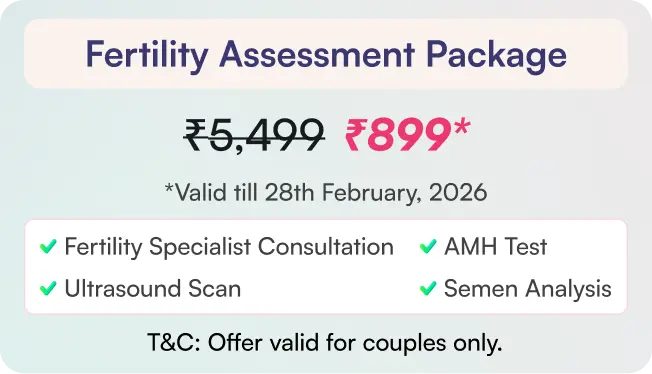
Typically, doctors grade embryos at two key developmental stages:
Day 3 (Cleavage Stage): At this stage, the embryo consists of a small number of cells called blastomeres. Grading focuses on:
Number of Cells: Ideally, a day 3 embryo should have 6 to 10 cells.
Cell Appearance (Morphology): This checks the similarity in cell sizes and the number of cell fragments. Lower fragmentation and evenly sized cells are preferred.
Grading Systems: Doctors have different ways to grade. They often use numbers from 1 to 4 or letters A to D. A higher number or an earlier letter shows better quality.
Day 5-7 (Blastocyst Stage): By day 5 or 6, the embryo develops into a blastocyst, which has a more complex structure. Grading at this stage uses the Gardner grading system and assesses three components:
Blastocyst Expansion (Grade 1-6): This shows how big the blastocyst is and its level of expansion. Higher numbers indicate more advanced expansion and hatching.
Inner Cell Mass (ICM) Quality (Alphabetical Grade A-C): The ICM will develop into the fetus. Grade A is the best (many tightly packed cells), while Grade C is the poorest (very few cells).
Trophectoderm Epithelium (TE) Quality (Alphabetical Grade A-C): The TE will develop into the placenta. Grade A is the best (many cells forming a cohesive layer), while Grade C is the poorest (very few cells).
How is Embryo grading done?
Embryo grading is an important part of IVF. Selecting the best embryos for transfer increases the likelihood of a successful pregnancy.
Grading occurs at two primary stages: day 3, which is the cleavage stage, and days 5 to 7, during the blastocyst stage. Each stage uses different criteria, with higher grades indicating better quality. Grades range from Grade 1 (Excellent) to Grade 4 (Poor). Grade 4 has too few or too many cells. It also features uneven cell sizes, moderate fragmentation, and heavy fragmentation. Even though the embryo is of poor grade, after implantation, there will be no abnormalities seen in the baby’s growth. The grades are only for the outer appearance of the embryo, but not for the level of genes.
The goal is to raise the chances of a successful pregnancy. We evaluate:
- The number of cells
- The appearance of the cells
- The uniformity of cell sizes
- Any fragmentation present
- Whether multinucleation is present
Why is the grading of embryos important?
Embryo Grading in the IVF Process is important due to the following reasons:
Prioritizing Embryos for Transfer: Grading embryos helps us choose the ones most likely to implant successfully based on their visual traits. Higher-grade embryos are selected for fertilization. These embryos are fertilized with high-quality sperm of the male partner to improve pregnancy chances.
Choosing Embryos for Freezing: We pick higher-quality embryos for cryopreservation. This way, we can use them for frozen embryo transfers (FETs) if the first cycle doesn’t work.
Implantation Potential Prediction: Higher embryo grades result in better chances for implantation and live births. However, grading is not a definitive predictor of success.
Informing Patients: Understanding grading allows patients to feel more confident about their treatment.
Research and Quality Control: We use embryo grading data for quality control. This data also plays a key role in communication between doctors.
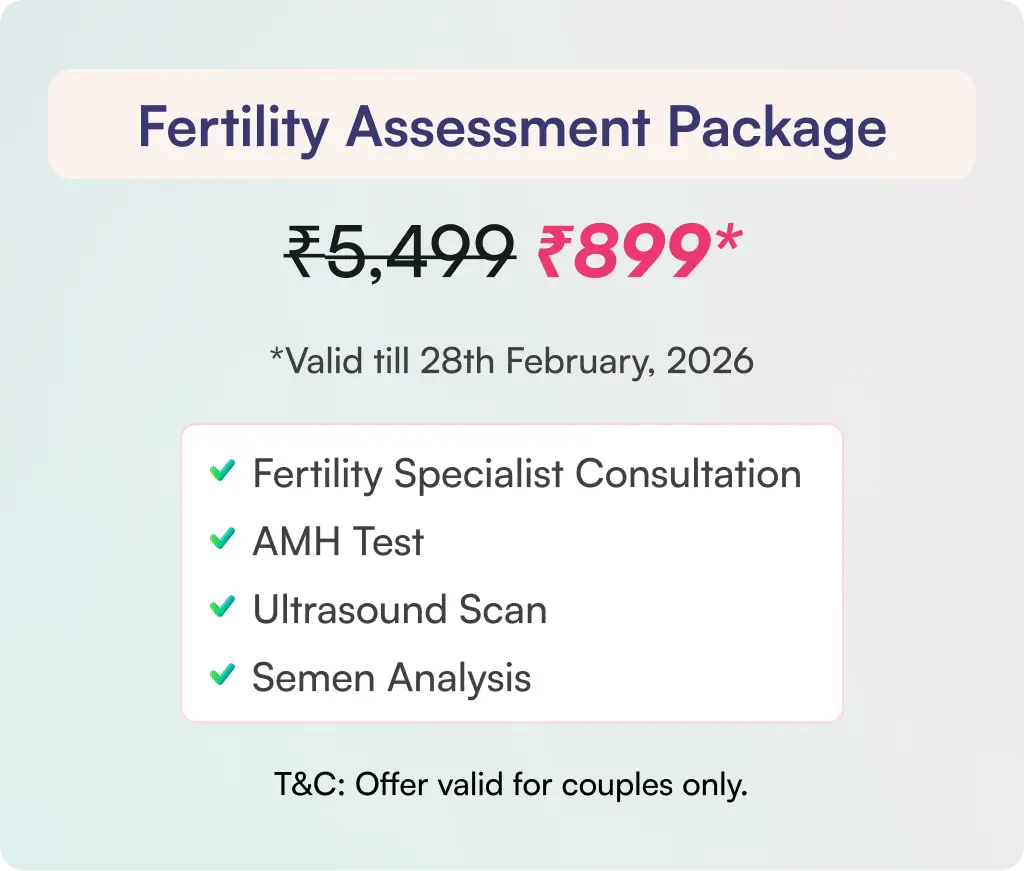
IUI: An Affordable Infertility Treatment
- IUI is less expensive and is less invasive, especially for unknown causes, and it helps place healthy sperm closer to the egg. IUI procedure is selected in particular situations such as:
- Works on thick or unfriendly cervical mucus. It can support irregular or absent ovulation, especially when used with ovulation-inducing medicines.
- Increases the likelihood of getting pregnant when endometriosis is mild.
- Fertility experts suggest trying 3 IUI cycles before IVF. This method will work great for women under 35 who face mild to moderate fertility problems.
Success Rates of IUI:
The success rates of IUI vary depending on several factors, including:
- Age of the woman: Success rates drop as maternal age rises, especially after 35.
Under 35: 10-20% per cycle
35-39: 10-15% per cycle
40 and over: 5-10% per cycle
- Sperm quality: Although IUI may help in mild male infertility, IVF is a better choice if sperm motility or count is very low, as this may significantly impact the success rates.
- Number of IUI cycles: The cumulative success rate increases with multiple IUI attempts. Around 60-80% of successful IUI pregnancies occur within 3-6 cycles.
What are the treatment options when IUI fails?
If IUI (Intrauterine Insemination) isn’t successful, you can look into laparoscopy or IVF (In Vitro Fertilization). They focus on different areas and play unique roles in your fertility journey. Here’s how they relate when IUI is unsuccessful:
Laparoscopy After Failed IUI
Purpose: Laparoscopy is a minimally invasive surgery. It helps doctors see the pelvic organs, like the uterus, fallopian tubes, and ovaries. It’s primarily a diagnostic and sometimes therapeutic tool.
When it might be considered after a failed IUI
Unexplained Infertility: If we don’t know the cause before IUI, laparoscopy might uncover some issues. It can detect mild endometriosis, pelvic adhesions, or minor tubal issues that might have affected IUI success.
Suspected Endometriosis: If you have signs or symptoms of endometriosis, laparoscopy is the best way to diagnose and may help treat it.
Tubal Issues: HSG (hysterosalpingogram) checks if the tubes are open. Laparoscopy gives a closer look and can fix small blockages or adhesions near the tubes.
IVF after failed IUI
Purpose: IVF is a type of assisted reproductive technology (ART). It involves getting eggs, fertilizing them outside the body, and transferring the embryos into the uterus. It bypasses many natural barriers to conception.
When it’s the typical next step after a failed IUI:
- Multiple Failed IUI Cycles: If 3 to 4 IUI cycles don’t work, especially for women over 35 or with known infertility, IVF is often the next step. It often has better success rates.
- Significant Male Factor Infertility: When sperm quality is very low, IVF with ICSI can directly inject sperm into the eggs.
- Tubal Factor Infertility: If your fallopian tubes are blocked or damaged, IVF is often the best option. It completely bypasses the tubes.
- Endometriosis: Laparoscopy can help manage endometriosis. IVF is often more successful for women facing moderate to severe challenges in getting pregnant.
- Advanced Maternal Age or Diminished Ovarian Reserve: IVF works better than IUI in these situations.
- Unexplained Infertility: If IUI isn’t successful and no problems appear, IVF may address hidden issues with fertilization or implantation.
- How it helps after a failed IUI: IVF improves your chances of getting pregnant. It supports fertilization and assists with embryo implantation.
- Success Rates: IVF usually has higher success rates per cycle than IUI. However, age and the cause of infertility still play a major role.
The Decision-Making Process
After a failed IUI, your fertility specialist will help decide between laparoscopy and IVF. You might also consider more IUI cycles. They will consider:
- Your age and ovarian reserve.
- The initial diagnosis and any potential reasons for IUI failure.
- The number of IUI cycles attempted.
- The seriousness of any known or suspected underlying issues, such as endometriosis or tubal problems.
- Semen analysis results.
- Your personal preferences and financial considerations.
After several failed IUI cycles or major infertility issues, the next step is often IVF. Laparoscopy may be used before IVF in certain cases. It helps find or fix problems that may impact IVF success or natural conception. However, it’s not a standard step after IUI failure.
It’s important to have a consultation with your fertility doctor. This way, you can identify the best next steps for your specific situation.