In the field of assisted reproductive technology, two commonly utilized fertility procedures are IVF (In Vitro Fertilization) and ICSI (Intracytoplasmic Sperm Injection). Both procedures assist couples dealing with infertility, but the differences between IVF and ICSI differ in how the sperm fertilizes the egg.
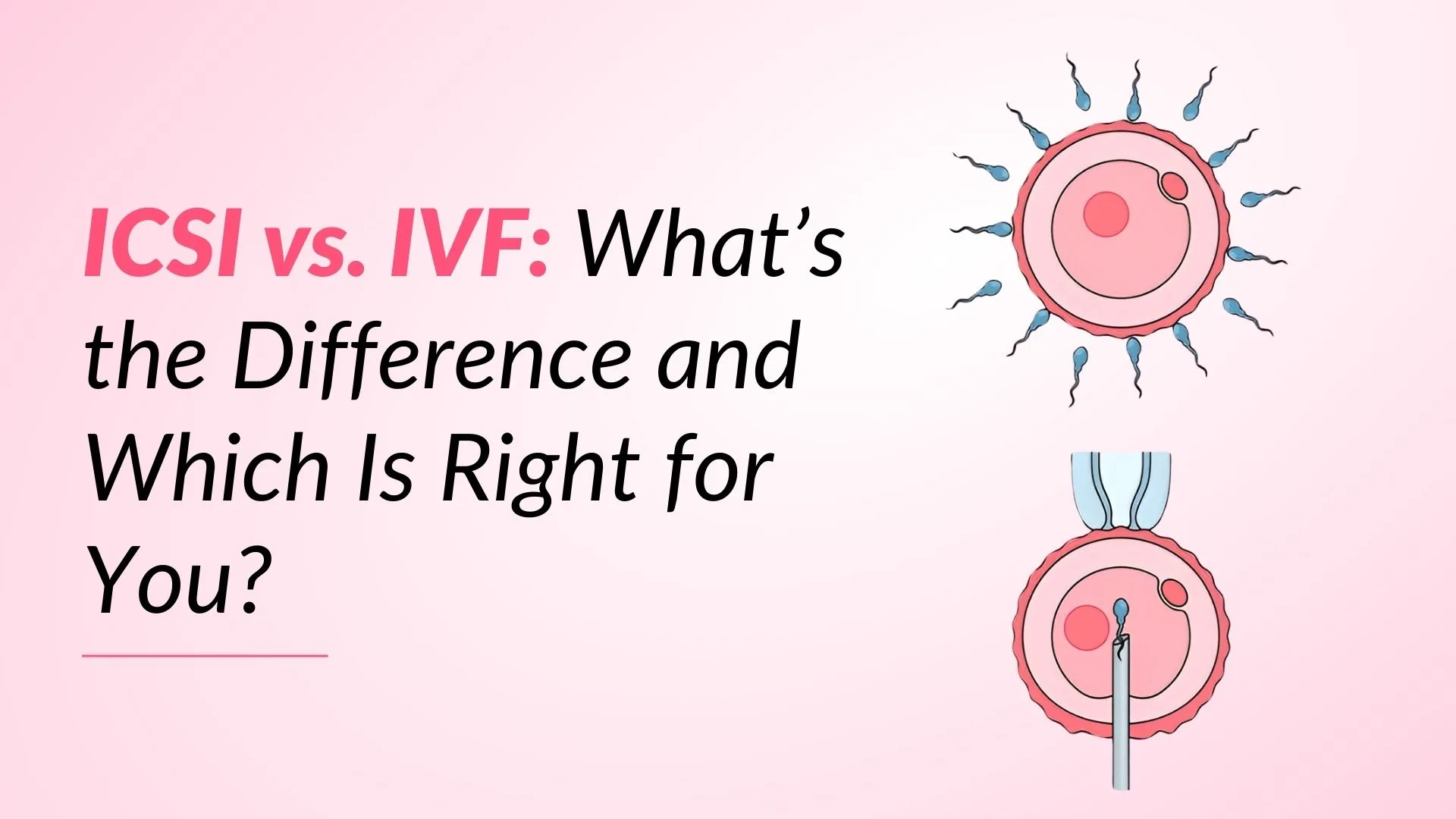
The main difference between IVF and ICSI is that in IVF, sperm fertilizes the egg naturally in a lab dish, while in ICSI, a single sperm is directly injected into the egg to ensure fertilization. The decision between IVF vs. ICSI is based on factors such as sperm quality, egg health, and underlying reproductive difficulties. Understanding their differences will help you decide which option is ideal for your path to parenthood.
What is In Vitro Fertilization (IVF)?
The most popular type of assisted reproductive technology is in vitro fertilization (IVF), which is used to manage patients who are having problems conceiving. The phrase ‘in vitro’ refers to the fertilization of oocytes in a laboratory, whereas normally, oocytes mature in vivo in the ovary, and embryos grow into pregnancy in the uterus.
What is Intracytoplasmic Sperm Injection (ICSI)?
Intracytoplasmic sperm injection, is typically used to overcome inadequate or absent fertilization in couples with abnormal semen parameters, but it is also sometimes combined with other assisted reproductive technologies to address various causes of infertility.
Intracytoplasmic sperm injection (ICSI) is a method of inserting a single sperm directly into an egg.
What are the Differences Between IVF and ICSI?
IVF (in-vitro fertilization) and ICSI (intracytoplasmic sperm injection) are assisted reproductive treatment (ART) treatments that fertilize eggs outside of the body. The key difference between IVF and ICSI is that IVF relies on natural sperm selection, whereas ICSI manually injects a single sperm into the egg to aid fertilization. IVF is utilized for female and unexplained infertility, while ICSI is used when there is a male cause of infertility. IVF (In Vitro Fertilization) involves combining sperm and eggs in a lab dish, enabling fertilization to occur spontaneously, whereas ICSI (Intracytoplasmic Sperm Injection) injects a single sperm directly into an egg to ensure fertilization. Both technologies are part of assisted reproductive technology, although they take different approaches to fertilization.
Risks During IVF
IVF increases the risk of certain health complications. These risks range from the short term to the long term. Before beginning IVF, it’s crucial to be aware of the potential complications you may encounter.
- Adverse effects of medicine
- Multiple births
- Ectopic pregnancy
- Ovarian hyperstimulation syndrome (OHSS)
- Risk of miscarriage and birth defects in elderly women
Risks During ICSI
Children conceived with ICSI have a higher absolute chance of the following conditions:
- Multiple gestation and its associated complications
- Congenital abnormalities (particularly genitourinary problems)
- Epigenetic syndromes (such as Beckwith Wiedemann)
Success Rates: IVF and ICSI
The success rates for IVF and ICSI vary depending on age, egg quality, and fertility issues. ICSI may help couples with severe male infertility, such as low or poor sperm motility, but IVF is effective when sperm quality is normal. In general, ICSI and IVF success rates are similar, but ICSI has slightly greater fertilization rates, especially for male infertility, but overall, pregnancy and live birth rates are similar. Although ICSI has a slightly higher risk of embryo defects, both techniques have comparable overall pregnancy success rates when performed under optimum conditions.
For a more accurate prediction of your timeline, try our IVF Due Date Calculator to plan your next steps
Cost Of IVF and ICSI Treatment
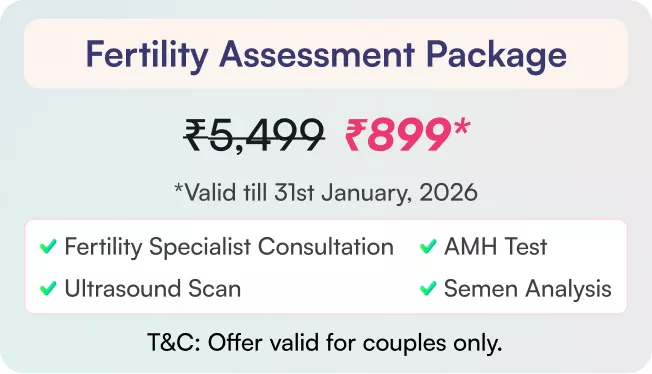
The cost of IVF and ICSI varies according to location, reputation of the fertility centers, and extra procedures needed. IVF normally costs between ₹150,000 to ₹225,000 per cycle. This comprehensive package includes ICSI if required, with no additional charges for the specialist sperm injection procedure. Insurance coverage varies, and additional fees for medications, embryo freezing, and genetic testing can increase overall costs. It’s essential to compare fertility centers and financing alternatives to discover the best deal for your budget.
When is ICSI recommended over IVF?
Compared to IVF, ICSI has a greater success rate. ICSI is preferred to IVF in the following situations:
1. Severe Male Infertility: Low sperm count, poor motility, or irregular sperm shape.
2. Previous IVF Failure: If fertilization has not occurred in previous IVF rounds.
3. Frozen Sperm Use: When using previously frozen or surgically extracted sperm.
4. Low Egg Count or Quality: Ensures fertilization using a restricted quantity of eggs.
5. Genetic Testing Requirements: If preimplantation genetic testing (PGT) is necessary, ICSI lowers the chance of sperm contamination.
6. Unexplained infertility
7. Blockages preventing ejaculation
8. Male partner with erection and ejaculation difficulties
9. A failed vasectomy reversal
Which Treatment is Right for You?
When considering ICSI vs. IVF , it’s essential to evaluate individual fertility factors, as ICSI may be more effective for couples facing male infertility challenges. Depending on your unique fertility issues, you can choose between IVF and ICSI:
- If sperm quality is normal and fertilization can happen naturally in the lab, IVF is better.
- When using frozen or surgically extracted sperm, severe male infertility, or prior IVF failure, ICSI is advised.
- ICSI may increase the likelihood of fertilization if egg quality or quantity is a concern.
- A fertility professional can help you choose the best course of action because both treatments have comparable success rates for getting pregnant.
- ICSI is often preferred for unexplained infertility, where standard IVF has failed without a clear reason.
- Couples undergoing genetic testing (PGT) may benefit from ICSI, as it ensures that only a single sperm fertilizes the egg, reducing contamination risks.
The decision of ICSI vs. IVF ultimately depends on specific fertility issues, as ICSI provides a targeted approach for fertilization, while IVF offers a broader option for those with varying fertility challenges.
Conclusion
The best option will rely on specific factors, including sperm quality, egg health, and past fertility history, but both IVF and ICSI are successful fertility procedures. While ICSI is best suited for couples with severe male infertility or a history of unsuccessful fertilization attempts, IVF is appropriate for couples with normal sperm parameters. The two treatments have comparable success percentages, and other aspects like price, genetic testing, and medical history should be considered. In the debate for ICSI vs. IVF , it’s critical to consult a fertility doctor to evaluate which treatment is best for your specific reproductive needs and circumstances.