Understanding the Fertility Timeline
Thinking about starting or growing your family? Have you ever wondered about the timeline; how long should it take to conceive? It would be very helpful for the couple to understand the typical fertility journey and the factors that may impact it. Discussing this topic in detail can help manage expectations and empower you to take proactive steps when needed.
Struggling to conceive? Check our IVF Treatment Cost and Success Rates to plan your journey.
The Average Time It Takes Healthy Couples to Conceive (Up to 12 Months)
Even for the healthy couples who engage in regular and unprotected intercourse, conception may not be successful. Almost 80% of couples become pregnant during the first year of trying. There is a brief window of time throughout each menstrual cycle for fertilisation. There are various ideal conditions for conception to take place that include:
- Ovulation: The release of a mature egg from the ovary.
- Sperm viability: Healthy and mobile sperm that can reach and fertilize the egg should be available.
- Timing of intercourse: Having intercourse during the fertile window of the female partner, plays a leading role.
- Overall health: General health and reproductive health play an important role for successful conception.
If you’ve been trying to conceive for about 3 months without success, don’t be discouraged. Patience is very important, but understanding when to seek a fertility specialist is essential. If you’re under age 35 and haven’t conceived after 12 months or 35 or older and haven’t conceived after 6 months, then it is time to consult fertility experts.
How age impacts fertility (especially for women over 35)
Age is an important factor that not only impacts fertility, for women, while men’s fertility also declines with age, the impact is generally more in women. Let us understand these factors:
Impacting women’s fertility
- Women’s fertility decreases with age, leading to a decrease in egg quality.
- Older eggs are more likely to have genetic abnormalities, increasing the risk of miscarriage.
- Women’s menstrual cycles may become shorter, reducing the fertile window every month.
- The likelihood of developing fertility-affecting conditions increases with age.
Impacting men’s fertility
- Sperm quality declines with age.
- Increased risk of erectile dysfunction and sexual health issues.
- Potential impact on conceiving ability due to decline in sperm count or increase in sperm related issues.
Proactively discussing your problems with a doctor can optimize chances of natural conception and advice from fertility specialists is needed.
Importance of tracking ovulation and timing intercourse
Understanding your menstrual cycle and identifying your fertile window is very important for successful conception. By planning timely intercourse around ovulation, you can increase the chances of fertilization. An egg typically fertilizes 12-24 hours after it’s released, while sperm can survive up to 5 days in the female reproductive tract. Ensuring the availability of sperm at the time of egg release increases the probability of sperm meeting the egg increases the chances to conceive.
Effective ways to track ovulation
- Understanding menstrual cycles helps predict ovulation.
- Tracking temperature at rest can identify a slight rise after ovulation.
- Ovulation Predictor Kits (OPKs) can be used to detect sudden increase in luteinizing hormone (LH) which implies ovulation has happened.
- Observing changes in cervical mucus provides clues about ovulation.
Is 3 Months Without Pregnancy Normal?
If you don’t conceive after three months of trying, it’s normal for healthy couples under age 35. Doctors generally recommend continuing natural fertility for at least six months to one year before recommending extensive testing. It’s important to understand the typical timelines and expectations for fertility in healthy couples.
Stats: percentage of couples who conceive within 3, 6, and 12 months
The average time to get pregnant by age is generally limited, but for individuals aged 21-24, there is a 57% chance of conception within 6 menstrual cycles and a 71% chance within a year. For women aged 25-27, there is a 59% chance of conception within 6 cycles and a 79% chance within 12 cycles. These figures are based on generalized data and should be taken with caution.
Differences between men’s and women’s fertility timelines
Women’s Fertility Timeline:
- Highest fertility in late teens and early twenties.
- Fertility declines after age 35, increasing pregnancy complications.
- Menopause around age 50, marking the end of reproductive years.
Men’s Fertility Timeline:
- Continuous sperm production from puberty.
- Gradual decline in sperm quality and quantity with age.
- Highest fertility in late teens and early twenties.
- Gradual decline after age 35, increasing risk of genetic abnormalities.
Common Reasons for No Pregnancy After 3 Months
A. Female-related causes
Irregular ovulation:
- Regular and predictable ovulation is very important for natural conception.
- Irregular or absent ovulation reduces the availability of egg for fertilization.
- Stress, weight changes, and underlying medical conditions impact ovulation.
Polycystic Ovary Syndrome (PCOS):
It is a common hormonal disorder that affects ovulation.
- Irregular or absent periods due to infrequent or absent ovulation.
- The hormonal imbalance due to small cysts on the ovaries affecting ovulation.
- Elevated levels of androgens (male hormones) can interfere with the development and release of eggs.
Thyroid disorders:
The thyroid gland plays a vital role in regulating many bodily functions, including the menstrual cycle and fertility. Both an overactive thyroid (hyperthyroidism) and an underactive thyroid (hypothyroidism) can disrupt ovulation and make it harder to conceive.
Endometriosis:
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus. This can affect fertility by interfering with the fertilized egg implanting in the uterus.
- Hormonal imbalances: Beyond specific conditions like PCOS and thyroid disorders, other hormonal imbalances can impact ovulation and the ability to get pregnant. These imbalances can involve various hormones, including:
- Progesterone: If progesterone levels are low, the egg may not be able to attach properly, leading to difficulty conceiving.
- Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH): The imbalance these hormones may impact egg release and ovulation.
- Prolactin: High levels of this hormone can sometimes interfere with ovulation.
B. Male-related causes
- Low Sperm Count (Oligospermia): This refers to having a low number of sperm in the semen, which makes successfully fertilizing the egg decrease.
- Poor Sperm Motility (Asthenozoospermia): Even with a normal sperm count, if a significant percentage of the sperm are unable to move properly (progressive motility), they may not be able to travel through the female reproductive tract to reach the egg.
- Absence of Sperm (Azoospermia): Sperm are needed to fertilize egg and achieve pregnancy naturally. If there are no sperm in the semen, natural conception isn’t possible.
- Varicocele: It is an enlargement of the veins within the scrotum. It can impact fertility by increasing the temperature of testicles or causing backflow of blood.
C. Lifestyle and Environmental Factors
Optimizing these factors together can create a more favourable environment for conceiving. Let’s explore some key lifestyle elements that play a crucial role for both partners
- Stress: In today’s fast-paced world, stress has become almost commonplace. High stress levels can disrupt the menstrual cycle, leading to irregular ovulation in woman. Stress can affect sperm production, motility, and morphology in men. It can also impact libido, making conception more challenging.
- Poor diet: Insufficient vitamins and minerals can impact women’s ovulation, egg quality, and uterine environment while it can affect men’s sperm production, motility, and overall health. A balanced diet rich in fruits, vegetables, whole grains, and lean protein is crucial for healthy hormones and reproductive function.
- Alcohol, smoking, and caffeine: Alcohol disrupts hormone levels, affecting ovulation and sperm production. Caffeine consumption is linked to reduced fertility, especially for women.
- Weight issues (overweight or underweight): Maintaining a healthy weight is crucial for optimal fertility in both men and women. Obesity can lead to hormonal imbalances like PCOS, affecting ovulation, while underweight can disrupt the menstrual cycle and ovulation. In men, obesity can lower testosterone levels, decrease sperm count, and increase the risk of erectile dysfunction.
- Lack of physical activity or excessive exercise: Physical activity enhances hormone balance and reduces stress, promoting fertility. However, a sedentary lifestyle can lead to weight gain and poor health, while excessive exercise can cause hormonal imbalances, irregular periods in women.
What You Can Do After 3 Months of Trying
While it can take time for conception to occur, there are proactive steps you can take to better understand your cycles, optimize your health, and improve your fertility.
A. Track your cycle:
Ovulation prediction tools and apps can detect raising levels of luteinizing hormone (LH), while fertility apps track periods and symptoms. Basal Body Temperature helps identify ovulation patterns over multiple cycles. Raise in hormone levels during ovulation can cause changes in cervical mucus, increased libido.
B. Optimize your lifestyle:
- Balanced diet with fertility-friendly nutrients (zinc, folate, vitamin D):
- Daily habits significantly impact overall health, including reproductive health.
- Focus on a diet rich in fruits, vegetables, whole grains, and lean protein.
- Include foods rich in Zinc (crucial for sperm production and ovulation), folate (essential for preventing neural tube defects and egg health), vitamin D (low levels lead to fertility issues) and foods rich in antioxidants (protect eggs and sperm), inositol (especially for PCOS problems).
- Stress management that includes yoga and meditation can help calm the mind and body, while therapy or counselling can provide emotional support. Engaging in enjoyable activities and incorporating relaxation time are also beneficial for mental strength that indirectly improve your fertility.
When to See a Fertility Specialist
Age is one of the most significant factors influencing fertility for both men and women, particularly for women due to the natural decline in egg quality and quantity over time. Here are the generally recommended timelines for seeking help from a fertility specialist based on a woman’s age:
Women under 35: after 12 months: For women under the age of 35 and have been actively trying to conceive for one year without success, it’s generally recommended to consult a fertility specialist. While many couples conceive within this timeframe, seeking evaluation after 12 months allows for timely identification and management of any underlying issues.
Women over 35: after 6 months: For women aged 35 and older, the timeline for seeking help is shorter. Due to age-related decline in fertility, it’s advisable to consult a fertility specialist after six months of actively trying to conceive without success. Earlier evaluation is very important in this age group to improve the chances of successful treatment.
Benefits of early testing: If a woman experiences irregular menstrual cycles, very long or short cycles, or has been diagnosed with conditions like Polycystic Ovary Syndrome (PCOS) known to affect ovulation, seeking help earlier will be beneficial.
What to expect during an initial fertility evaluation: A specialist will gather detailed medical history, perform a physical examination, recommend initial testing and develop a personalized treatment plan. This may include blood tests for women and ultrasounds for men. The specialist will also discuss potential causes and treatment options.
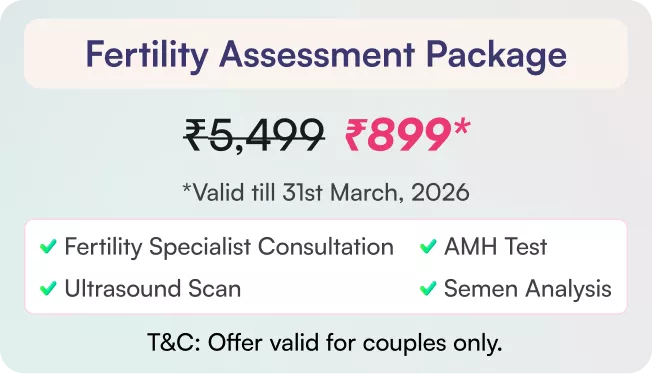
Medical Tests to Explore
- For women: Identifies presence of ovarian cysts, assesses follicle count, and detects masses or structural abnormalities. Evaluates the uterus, uterine lining, fibroids and other structural issues. Can be performed trans-abdominally or transvaginally, with the doctor determining the most suitable method.
Common tests include FSH, LH, estrogen, and AMH, which indicates high FSH levels due to decline in ovaries and low LH levels indicating ovarian function issues. Ultrasound scan to visualize internal reproductive organs. HSG (hysterosalpingogram) test is done to check any blocks in fallopian tubes and abnormalities in the uterine cavity.
- For men: Semen analysis is primarily done to assess sperm health and viability, taken from ejaculation for 2-3 days. Hormonal tests are conducted to assess levels of key hormones like testosterone, FSH, LH, prolactin, and estradiol. Scrotal ultrasound is done for specific concerns identified during physical exams or other tests.
Alternative Options
If there are any underlying medical conditions identified by fertility specialist, the recommended treatment options are IUI, IVF:
- Intrauterine Insemination (IUI) involves placing sperm into the uterus during ovulation, suitable for mild infertility or unexplained infertility.
- In Vitro Fertilization (IVF) involves retrieving eggs from the ovaries, fertilizing them in a laboratory, and transferring them back into the uterus.
Conclusion:
Understanding the fertility timeline is crucial for couples planning to start or grow their family. Healthy couples typically conceive within 12 months. Age impacts fertility, with women experiencing decreased egg quality and men experiencing declining sperm quality. Discussing with doctors may help you overcome issues and improve chances with early consultations.






























 No need to worry, your data is 100% safe with us!
No need to worry, your data is 100% safe with us!